Some blog posts may contain affiliate links and if you purchase products through these links I will earn a small commission at no additional cost to you. Thank you for your support!
Everything You Need to Know About Mastitis
For breastfeeding mothers, mastitis can be a concerning and uncomfortable condition that may arise unexpectedly. Understanding what mastitis is, its symptoms, and how to manage it is crucial for maintaining both your health and your ability to continue breastfeeding comfortably.
What is Mastitis?
Image featuring Amelia Nursing Crop Cami.
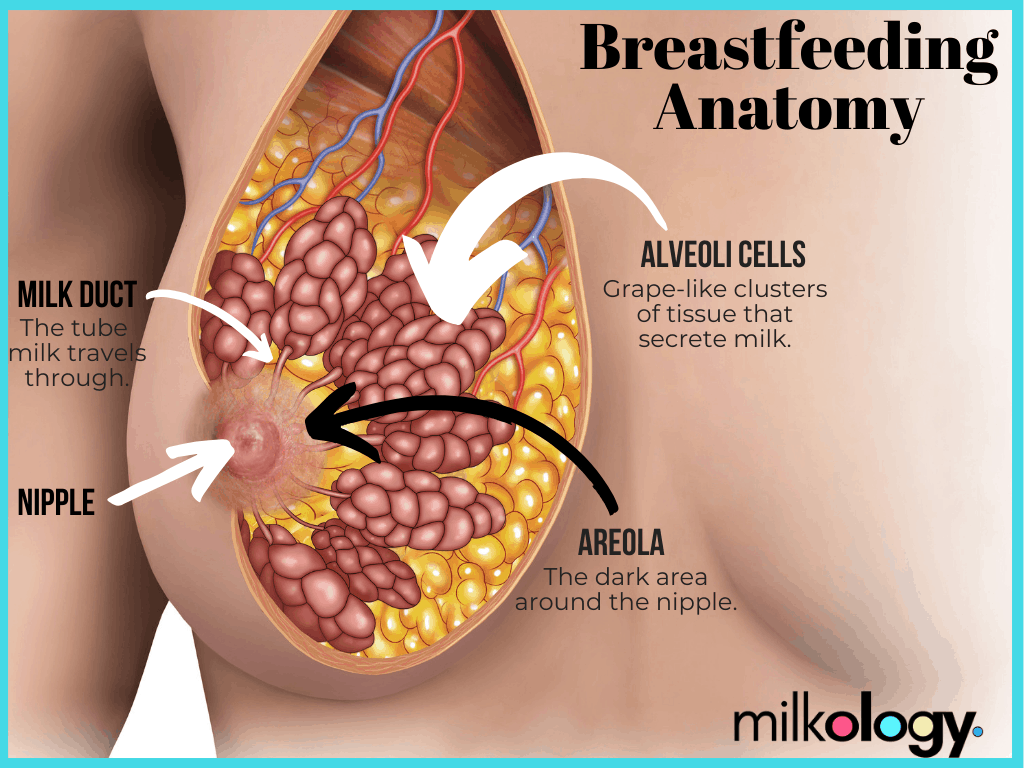
Mastitis can be defined as an infection or disruption in breast tissue, primarily caused by ductal narrowing, followed by inflammatory mastitis, if worsens, bacterial mastitis. Generally speaking, ductal narrowing that isn't addressed properly can be the leading cause in most cases of mastitis. Ductal narrowing refers to pressure surrounding the milk ducts which acts as the roadway for milk to exit the breasts.
What causes mastitis?
Hyperlactation, also known as oversupply, has been known to be a leading cause of mastitis. When milk ducts become restricted—typically due to irregular breastfeeding patterns, latch problems, or wearing tight clothing—the increasing pressure surrounding the milk ducts will exacerbate discomfort and increase chances of worsening symptoms such as pain, redness, swelling, and fever AKA onset mastitis.
Other contributing factors include:
- Exhaustion
- Weakened immune system
-
Stress (I know, it's hard to avoid stress or get much rest during the first weeks with a new baby at home!)
These factors can also contribute to the development of mastitis by making the body more susceptible to infection.
When addressing nipple trauma or visible damage, according to the Academy of Breastfeeding Medicine Protocol #36, The Mastitis Spectrum, there is no evidence to suggest that bacteria found outside of the breast tissue, at surface level, is to blame for mastitis.
Symptoms of Mastitis
Mastitis manifests with distinct symptoms that breastfeeding mothers should be aware of. Treating mastitis as early as possible can help prevent further complications. Typically, it begins with a localized area of the breast becoming red, swollen, and warm to the touch. This inflammation often leads to pain or tenderness in the affected breast, which may worsen during breastfeeding or between feedings. The breast may feel lumpy or have a hard, knot-like area due to blocked milk ducts.
Mastitis Symptoms To Look Out For:
- Breast Pain: One or both breasts may feel sore or tender to the touch.
- Redness and Heat: The affected area of the breast may appear red and feel warm.
- Swelling: The breast may swell, and the area affected may feel lumpy or hard.
- Fever and Chills: Some women may experience flu-like symptoms such as fever, chills, and body aches.
- Fatigue: Mastitis can cause general feelings of tiredness or malaise.
Image from Milkbar Breast Pumps
Mastitis Treatment
To effectively treat mastitis, follow these steps:
-
Continued Breastfeeding: Ensure frequent nursing sessions from both breasts to keep milk flowing and prevent another clogged milk duct. Generally speaking, frequent breastfeeding also helps prevent recurrent mastitis. Newer research shows that you don't need to add additional milk removal during mastitis, just continue as normal.
-
Iced Compresses: Cold compresses to the affected breast to help reduce swelling. Think of this process similarly to how you would treat a sprain ankle. Although heat will vasodilate and may worsen symptoms, this process has also shown to provide comfort for some patients. Considering a combination of both applications may be beneficial, but the newest protocol recommends cold.
-
Rest and Hydration: Get adequate rest and drink plenty of fluids to support your immune system's ability to fight the infection.
-
Pain Relief: Take over-the-counter pain relievers like ibuprofen to reduce sore breast discomfort and inflammation.
-
Consult Health Care Provider: If symptoms persist or worsen, seek medical advice promptly. They will likely conduct a physical exam of your infected breast to determine the best way to treat your specific condition. Oral antibiotics may be prescribed to treat the bacterial mastitis infection, and it's essential to complete the full course of antibiotic treatment as directed.
- Avoid Tight Bras: This is a good breastfeeding tip in general, but if you suspect a clogged duct or mastitis, it's essential that you choose a bra with some stretch. The Amelia Crop Cami and Ella Bralette are both great options for non-restrictive nursing and pumping bras.
Following these steps diligently can help manage mastitis effectively, ensuring a quicker recovery and allowing breastfeeding to continue smoothly.
Image Featuring Ella Bralette
Impact on Baby
Always check with your doctor, but it is almost always recommended to continue breastfeeding through mastitis. Infants may sense changes in their mother's behavior due to discomfort or fatigue from mastitis, impacting their feeding patterns and overall feeding experience. However, with proper management and continued breastfeeding, these effects are typically temporary and do not pose long-term health risks to the infant. Prompt treatment of mastitis ensures that breastfeeding can continue smoothly, benefiting both the mother and her baby's health.
Other Breast Infections to Look Out For:
While mastitis is a common breast infection among breastfeeding women, there are other conditions to be aware of:
-
Thrush: A fungal infection caused by Candida yeast, often characterized by persistent nipple pain and shiny or flaky skin on the nipple or areola.
- Milk Blebs: Also known as a milk blister, a milk bleb is a small, white or yellowish spot on the nipple that can cause pain and discomfort during breastfeeding.
Both thrush and milk blebs require proper diagnosis and treatment, which may include antifungal medications for thrush or techniques to clear milk blebs such as warm compresses or gentle massage. Awareness of these conditions and seeking timely medical advice can help ensure continued comfort and successful breastfeeding.
Here's My Take:
After breastfeeding, all three of my babies, I can say that I was very fortunate to never have to battle mastitis, but there are a few key factors to how I was able to avoid having it during my three different breastfeeding journeys.
1. I never skipped a nursing or pumping session.
I was constantly removing milk by either my baby nursing or a breast pump, so my breast tissue stayed soft. This included pumping or nursing every 2 to 3 hours until my babies were older and I could go longer between sessions. When traveling without my baby, my pumping sessions replaced nursing entirely but it was important to never skip at all.
2. I never wore tight restricting bras or underwires while breastfeeding.
It’s super important to wear something that has enough stretch to accommodate your growing breast tissue. If you put too much pressure on the milk ducks, it can cause inflammation, milk blebs, clogged ducts, and mastitis. My personal favorite bra of all time has been the Amelia pumping and nursing crop Cami. (See image.)
I have worn the Amelia bra almost every single day for my second and third babies. The fit and design of this pumping and nursing bra with no restrictive fabric or wires and plenty of breast coverage for my size, has hands down helped me avoid clogs and mastitis.
3. I addressed clogs immediately.
Whenever I felt the onset of a clog, I always practiced hand expression and breast massage to help the milk flow. I would address a clog immediately because the longer you wait the more likely you are to develop mastitis if the milk is not properly being removed. The protocol for clogs has also changed to follow the same as mastitis (iced compress), but one of my go to tools was a breast massager with the option of heat.
Although mastitis can be challenging, especially for new mothers navigating the joys and challenges of breastfeeding, it is typically manageable (or avoidable) with proper care and attention. Recognizing symptoms early and taking proactive steps like continued breastfeeding, rest, and hydration are key to recovering quickly.
Always consult with a healthcare provider if you suspect mastitis or have concerns about your breast health during breastfeeding. By staying informed and proactive, you can effectively manage (or avoid!!) mastitis and continue to enjoy the bonding experience of breastfeeding with your baby.









